Helping your patients make the right choice
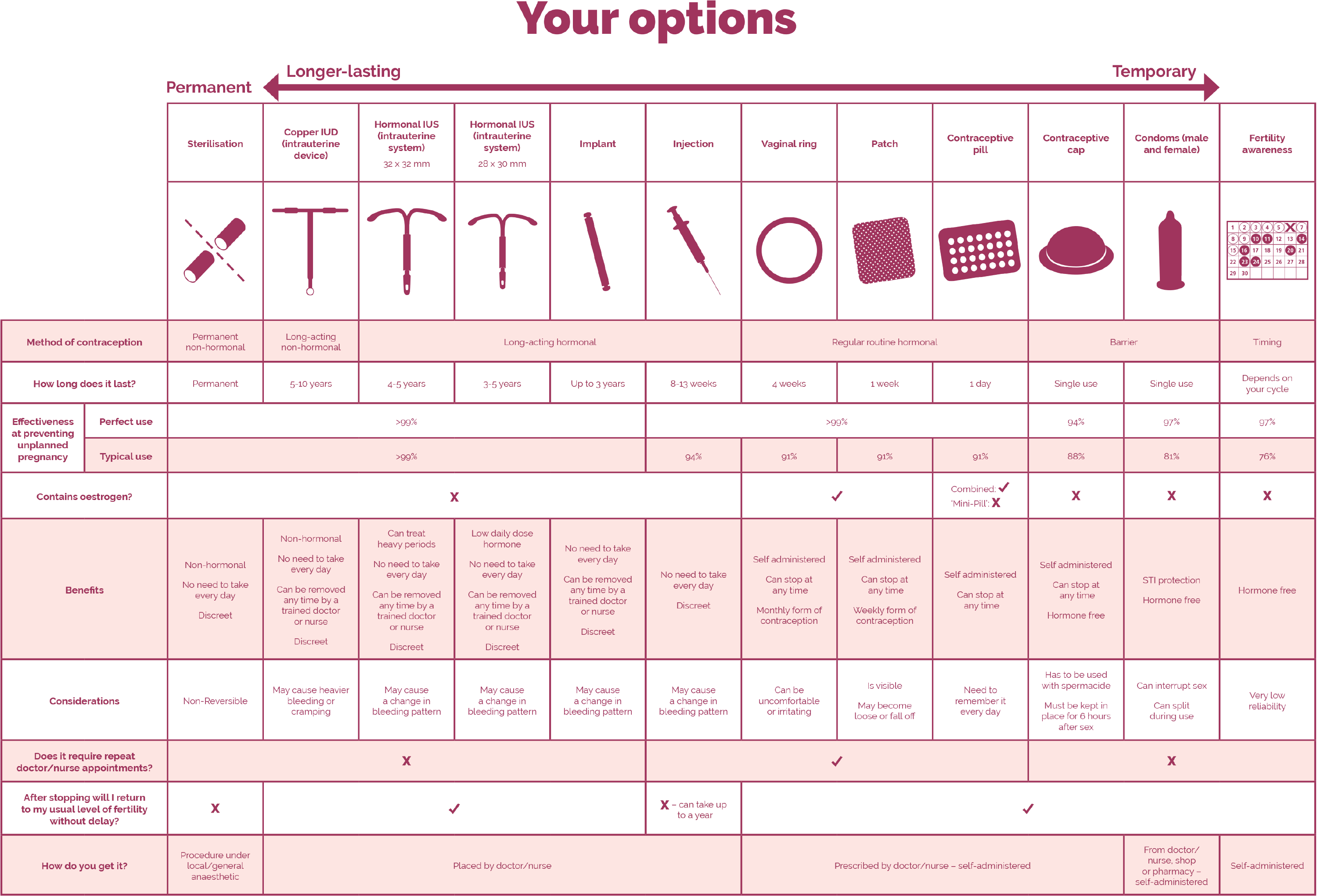
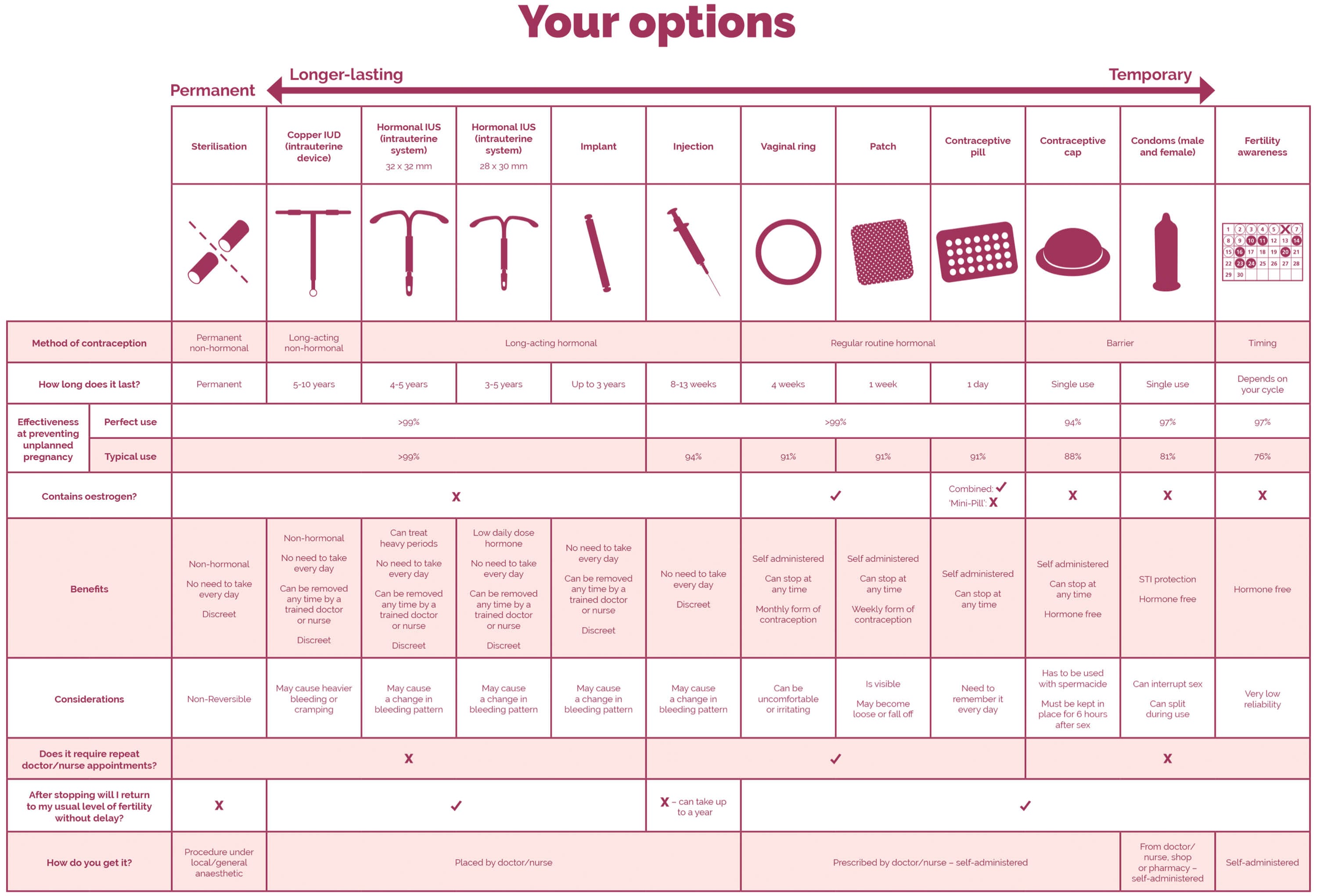
With recent research showing that almost a third of Irish women aged 17-45 have had sex in the past where contraception has failed, there is a clear need to offer the most effective contraceptive methods.1 In an on-line survey of 1,014 Irish females aged 17 to 45 years of age where they were asked about contraception, almost three quarters (73%) of those who have experienced a contraceptive failure in the past claim that they were using a condom / male sheath when the contraception failed.1 Whilst just over a third of women aged 17-45 have had sex in the past where the contraception failed, and this resulted in a pregnancy. 1Long-acting methods can be the most effective form of contraception because they do not rely on user compliance.2
Here you will find resources to guide conversations with your patients, helping to identify which is the most suitable contraception for them.
- The Contraception Conversation, Dublin Well Woman & Empathy Research, supported by an educational grant from Bayer. On-line survey conducted on the 10th-23rd March 2020 with 1,014 females aged 17-45 years. Available online from: https://wellwomancentre.ie/research-publications/ Return to content
- Cristobal I, et al. Eur J Obstet Gynecol Reprod Biol 2015;190:58–64. Return to content
Pill compliance is a common struggle for women1
For every 100 women that choose to take the pill this year, nine could become pregnant due to missed-pill moments.2 Long-acting methods such as intrauterine systems (IUS) offer birth control with the highest available efficacy and are one of the most effective contraceptive methods because their effectiveness is independent of user compliance.3
- Merki-Feld GS, et al. Eur J Contracep Reprod Health Care 2018:183–193. Return to content
- NHS. How effective is contraception at preventing pregnancy? - Your contraception guide [online]. Updated 30 June 2017. Available from: https://www.nhs.uk/conditions/contraception/how-effective-contraception/. Return to content
- Cristobal I, et al. Eur J Obstet Gynecol Reprod Biol 2015;190:58–64. Return to content

Choose an IUS that best meets her needs
| Jaydess®▼1 13.5 mg intrauterine delivery system (levonorgestrel) |
Kyleena®2 19.5 mg intrauterine delivery system (levonorgestrel) |
Mirena®3 52 mg intrauterine delivery system (levonorgestrel) |
|
|---|---|---|---|
| Indication | Contraception for up to 3 years | Contraception for up to 5 years | Contraception for up to 8 years. Treatment of idiopathic menorrhagia for up to 5 years. If symptoms have not returned after 5 years of use, continued use of the system may be considered. Mirena should be removed or replaced after 8 years at the latest. Protection from endometrial hyperplasia during estrogen replacement therapy for up to 5 years |
| Pearl Index (efficacy) | Year 1:0.41 3-years: 0:33 |
Year 1: 0.41 3-years: 0.33 |
Year 1: 0.2 Years 5: 0.144 Years 6-8: 0.28 |
| Contraceptive failure rate | 0.4% at 1 year 0.9% over 3 years |
0.2% at 1 year 1.4% over 5 years |
Year 1: 0.2% Years 1 to 5: 0.7% Years 6 to 8: 0.68 |
| Total levonorgestrel (LNG) content (mg) | 13.5 | 19.5 | 52 |
| Average in vivo LNG release rate over the first year of use | 8 μg/24 hours | 12.6 μg/24 hours2 | 20 μg/24 hours |
| % of women experiencing amenorrhoea and infrequent bleeding at 1 year post insertion | Amenorrhoea: 6% infrequent bleeding: 20% |
Amenorrhoea: 12% infrequent bleeding: 26% |
Amenorrhoea: 16% infrequent bleeding: 57% |
| T-frame size (mm) | 28 × 30 | 28 × 30 | 32 × 324 |
| Placement tube diameter size (mm) | 3.8 | 3.8 | 4.4 |
| Colour of monofilament threads | Brown | Blue | Brown |
| Differentiator in imaging techniques:silver ring | Improved visibility on ultrasound | Improved visibility on ultrasound | - |
- Bayer Ltd. Jaydess®▼13.5 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available online from: https://www.medicines.ie/medicines/jaydess-13-5-mg-intrauterine-delivery-system-32547/spc Return to content
- Bayer Ltd. Kyleena® 19.5 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available online from: https://www.medicines.ie/medicines/kyleena-19-5-mg-intrauterine-delivery-system-32621/spc Return to content
- Bayer Ltd. Mirena® 52 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available online from: https://www.medicines.ie/medicines/mirena-52mg-intrauterine-delivery-system-32902/spc Return to content
- Bayer Plc. Mirena® 52 mg intrauterine delivery system (levonorgestrel): Product Information. Bayer Australia Return to content
Recommendations
Reporting adverse events and quality complaints
If you want to report a side effect or quality complaint, please contact your health care professional (e.g. physician or pharmacist) or The Health Products Regulatory Authority, Reports can also be reported directly to Bayer through this link or by emailing directly on adr-reland@bayerhealthcare.com