Up to 8 years of highly effective contraception1
Mirena® a hormonal intrauterine system that provides contraceptive protection for up to 8 years and treatment of heavy menstrual bleeding (If symptoms have not returned after 5 years of use, continued use of the system may be considered. Mirena should be removed or replaced after 8 years at the latest.). It is inserted into the uterus and releases the hormone levonorgestrel in small doses (20 μg/24 hours) into the uterine cavity.
Mirena® has the broadest range of indications and the longest licensed duration of action for an IUS, offering:1
- 5 years of effective relief from HMB (If symptoms have not returned after 5 years of use, continued use of the system may be considered. Mirena should be removed or replaced after 8 years at the latest.)
- 8 years of contraceptive efficacy
- 5 years of endometrial protection
The local release of hormone ensures low systemic levels of levonorgestrel, meaning that the incidence of hormone-related adverse events is low.
Mirena® therapeutic indications1
- Contraception.
- Idiopathic menorrhagia. Mirena® may be particularly useful in women with idiopathic menorrhagia requiring (reversible) contraception.
- Protection from endometrial hyperplasia during oestrogen replacement therapy.
- Mirena® Summary of Product Characteristics Return to content
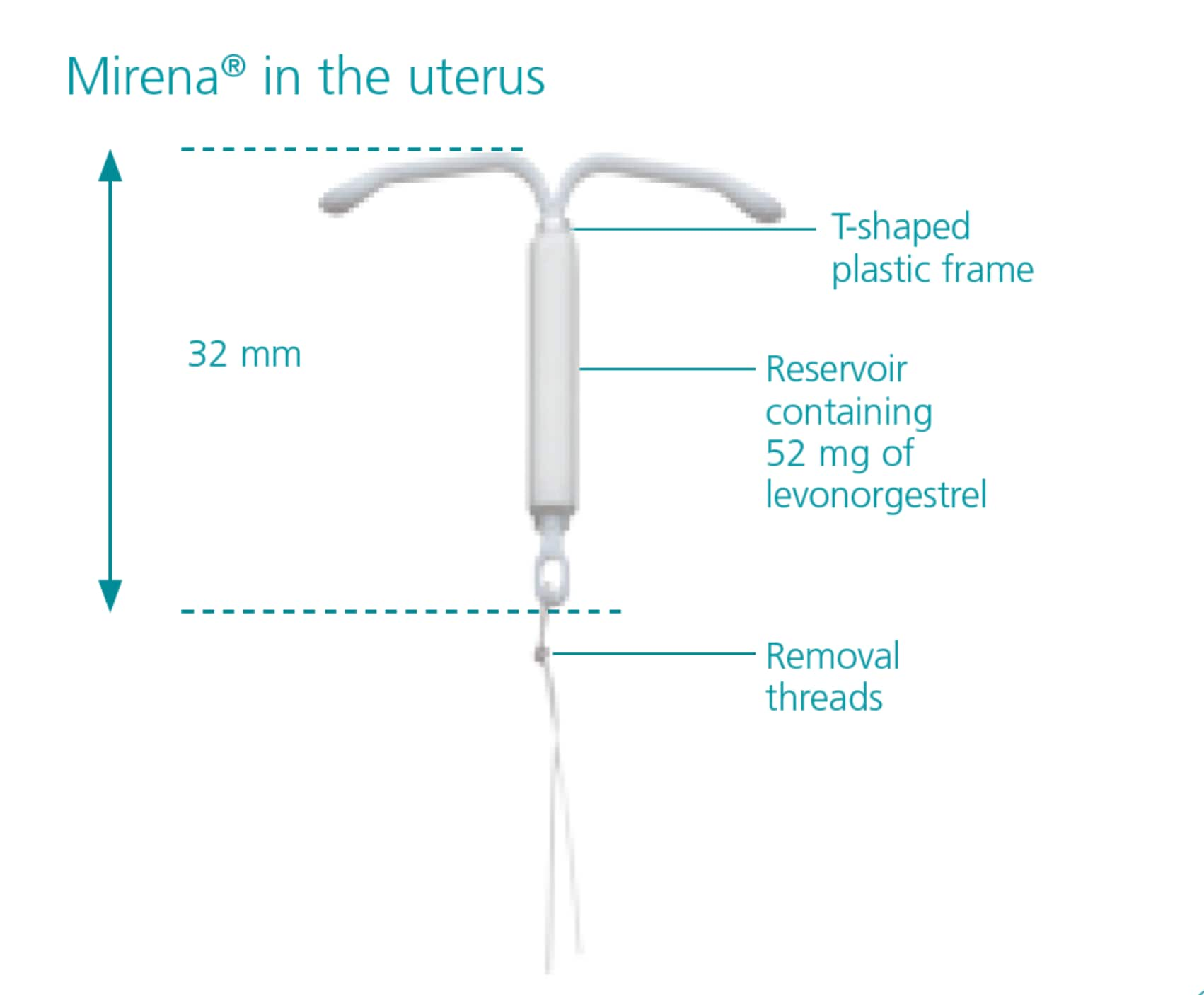
Mirena® opens out to a T-shaped plastic frame with a cylinder-shaped reservoir around the vertical arm of the frame. The reservoir contains the progestogen levonorgestrel.
The size of Mirena® is approximately 32 mm x 32 mm.1
- Bayer PLC. Mirena® product information. Bayer Australia, 2017 Return to content
Watch step-by-step video guidance on the preparation, insertion, removal and replacement of the Mirena® IUS here.
How does Mirena® work?
The contraceptive effect of Mirena® is based on a local effect of levonorgestrel:1
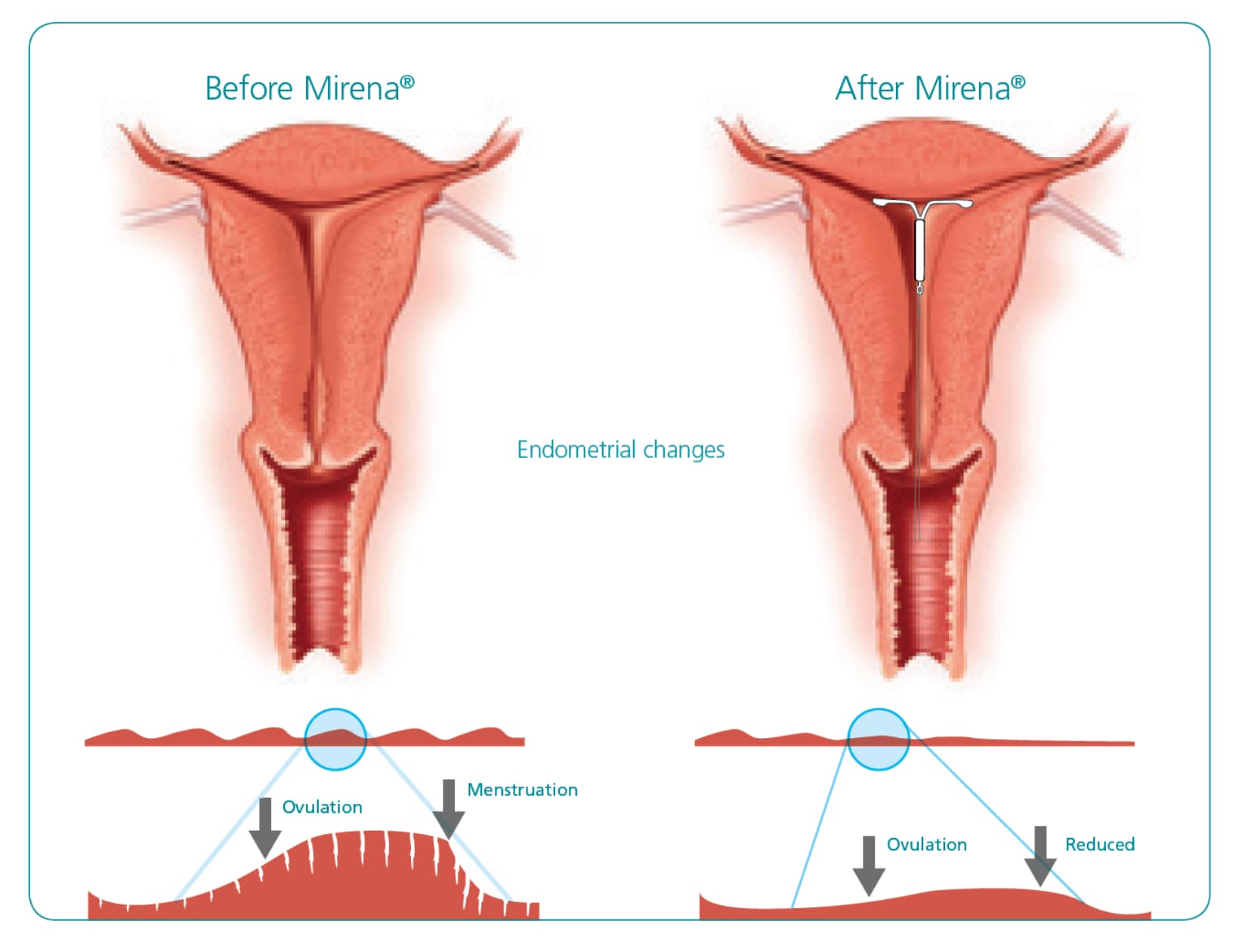
- The cervical mucus is thickened making it difficult for the sperm to get through to fertilise the egg.
- Normal sperm movement and function inside the uterus and ovarian tubes is inhibited.
- The growth of the lining of the uterus (endometrium) is reduced, which also makes menstrual blood loss much lighter and shorter.
Due to these changes in the endometrium, many women will have spotting and irregular bleeding during the first 3-6 months following the insertion of Mirena®. Thereafter, the strong suppression of the endometrium results in shorter and lighter periods.
Understanding the bleeding pattern is an essential aspect of counselling and appropriate patient education has been shown to promote continuation.2,3
Refer to the IUC myth busters for help in combating common patient concerns.
- Mirena® Product monograph, 9th edition, 2010. Return to content
- Peipert J, et al. Obstet Gynecol, 2011;117:1105–13 Return to content
- Madden T, et al. Contraception, 2013;88(2):243–249. Return to content
NICE recommends a levonorgestrel-releasing (LNG) IUS, like Mirena®, as a first-line option for heavy menstrual bleeding (HMB).1
Read the latest NICE clinical guidance on Heavy menstrual bleeding: assessment and management (2018)
- NICE guideline NG88. Heavy menstrual bleeding: assessment and management (November 2018). Available at: https://www.nice.org.uk/guidance/ng88.. Return to content
Mirena Prescribing Information
Wendy describes the impact of heavy menstrual bleeding on her life before and after Mirena®
- Xu L, et al. International Journal of Women’s Health. 2014;6:547–554. Return to content
- Romer T and Linsberger D. The European Journal of Contraception and Reproductive Health Care. 2009;14(6):391–398. Return to content
Mirena® is a trusted choice for you and your patients
Over 26 years
of clinical experience1
More than 270 clinical trials
and over 5000 peer-reviewed publications to date2
An estimated 43.7 million
insertions worldwide3
- Kailasam C and Cahill D. Patient Prefer Adherence. 2008; 2:293–302. Return to content
- PubMed www.ncbi.nlm.nih.gov/pubmed: search result (Mirena AND women). Last accessed 23 October 2017. Return to content
- Data on file. Mirena® Insertion data 2017. Bayer Healthcare. Return to content
Mirena®: Frequently asked questions
Below you will find answers to some commonly asked questions, which you may find useful when assessing appropriate contraceptive options for patients or counselling patients on contraception choice and Mirena® (52 mg intrauterine delivery system levonorgestrel).
Women who suffer from idiopathic menorrhagia or require endometrial protection during oestrogen replacement therapy may benefit from Mirena® (52 mg intrauterine delivery system levonorgestrel), which is indicated as a contraceptive option that prevents pregnancy and as a treatment option for both conditions.1
Mirena® is a long-acting reversible contraceptive device that may be particularly useful in women with idiopathic menorrhagia (also known as heavy menstrual bleeding) who also require (reversible) contraception.1 Mirena® would also be an option for a woman requiring the progestogenic component of hormone replacement therapy (HRT).
- Bayer Ltd. Mirena® (52 mg intrauterine delivery system levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/mirena-52mg-intrauterine-delivery-system-32902/spc. Return to content
Mirena is indicated for contraceptive use for up to 8 years, as a treatment for menorrhagia for up to 5 years (If symptoms have not returned after 5 years of use, continued use of the system may be considered. Mirena should be removed or replaced after 8 years at the latest.) and as protection from endometrial hyperplasia during oestrogen replacement therapy for up to 5 years. If the patient wishes to continue using the same method, it can be replaced by a new system at any time of the cycle at the same time, in which case no additional protection is required.1
- Bayer Ltd. Mirena® (52 mg intrauterine delivery system levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/mirena-52mg-intrauterine-delivery-system-32902/spc. Return to content
A recent study of more than 6,000 women showed that 73% across all age ranges (18–49) would consider long-acting reversible contraception (LARC) if provided with substantial information from their healthcare professional (HCP) on this method (compared with 38% estimated by HCPs).2
In general, fewer patients are uncomfortable with the idea of having a foreign device inside their bodies if they were previously aware of an LNG-IUS such as Mirena® (52 mg intrauterine delivery system levonorgestrel) vs those who were not aware. This highlights the importance of effective counselling to increase awareness and knowledge.3
A patient may feel reticent to have a Mirena® (52 mg intrauterine delivery system levonorgestrel) inserted, this could be due to the following myths and misperceptions:
- 'Fitting and removal will be painful'.
- Some patients may feel pain or have some bleeding during insertion or removal1
- Some patients may feel pain or have some bleeding during insertion or removal1
- 'The IUS will perforate and end up somewhere other than my uterus without me knowing'.
- Perforation occurs in less than 1 in 1000 women and can be detected by severe pelvic pain and continued heavy bleeding for more than a few weeks after insertion5
- Perforation occurs in less than 1 in 1000 women and can be detected by severe pelvic pain and continued heavy bleeding for more than a few weeks after insertion5
- 'I will suffer years of irregular bleeding'.
- The chance of irregular bleeding can happen in the first 3 - 6 months after insertion
- The chance of irregular bleeding can happen in the first 3 - 6 months after insertion
Women have other perceptions of IUS which it is important to counsel them around:
- 11% of women consider the hormone level to be very high4
- 30% of women are opposed to having something like a hormonal coil inserted in their body4
- 37% of women feel they don’t know enough about hormonal coils4
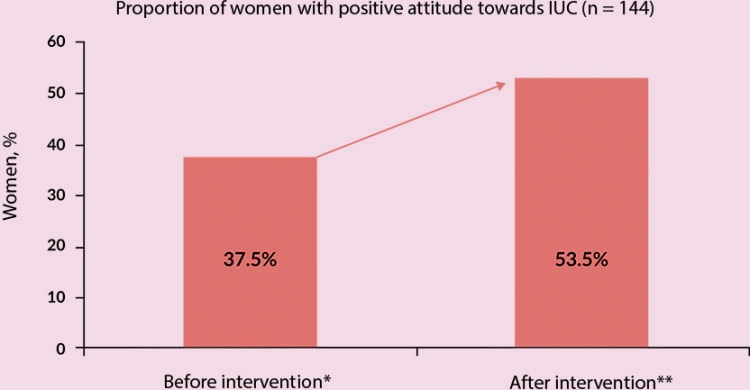
However, a study by Whitaker et al showed that adolescents and young women report a positive attitude towards intrauterine contraceptives before and after a 3-minute educational intervention counselling tool, which included information about IUS effectiveness, insertion and removal process, risks, benefits, costs, effect on fertility, menstrual effects, length of use, similarities and differences between types of IUSs available. Attitudes before and after the education intervention were assessed by questionnaire.6
- Bayer Ltd. Mirena® (52 mg intrauterine delivery system levonorgestrel): Summary of Product Characteristics Available from: https://www.medicines.ie/medicines/mirena-52mg-intrauterine-delivery-system-32902/spc Return to content
- Merki-Feld GS, et al. Eur J Contracept Reprod Health Care 2018;23:183–193. Return to content
- Peiper FJ, et al. Obstet Gynecol 2010;120:1291–1297. Return to content
- PULSE survey 2018 UK. Return to content
- gov.uk. Intrauterine contraception: uterine perforation—updated information on risk factors [online]. Updated 26 June 2015. Available from: https://www.gov.uk/drug-safety-update/intrauterine-contraception-uterine-perforation-updated-information-on-risk-factors Return to content
- Whitaker A, et al. Contraception 2008;78:211–217. Return to content
The intrauterine device Mirena® contains levonorgestrel 52 mg. Levonorgestrel is a well-established progestogen with antioestrogenic activity.1
The effect of hormonal contraceptives such as Mirena® may be reduced by medicines that increase the amounts of enzymes made by the liver. These include:1
- Medicines used to treat epilepsy
- Antifungal medicines (e.g. griseofulvin, fluconazole, itraconazole, ketoconazole, voriconazole)
- Certain antibiotics (rifampicin & macrolides [e.g. clarithromycin, erythromycin])
- Medicines used to treat HIV and Hepatitis C virus infections (so-called protease inhibitors and non-nucleoside reverse transcriptase inhibitors)
- Certain sedatives (called barbiturates)
- Medicines used to treat chest pain (angina) and/or high blood pressure
- Products containing St John’s Wort (a herbal remedy)
For a full list of medicinal interactions with Mirena® and contraindications, refer to the Summary of Product Characteristics.
- Bayer Ltd. Mirena® (52 mg intrauterine delivery system levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/mirena-52mg-intrauterine-delivery-system-32902/spc Return to content
Undesirable effects are more common during the first months after the insertion of Mirena® (52 mg intrauterine delivery system levonorgestrel) and subside during prolonged use.
In less than 1 in 10 women, common side effects of Mirena® include:1
- ovarian cysts
- painful periods
- weight gain
- depression, nervousness
- headache
- migraine
- abdominal, pelvic or back pain
- nausea
- acne
- increased growth of hair on the face and body
- reduced sex drive
- increased vaginal discharge
- inflammation of the vulva and vagina
- tender, painful breasts
- Mirena® expulsion
Very common undesirable effects (occurring in more than 10% of users) include uterine/vaginal bleeding including spotting, oligomenorrhoea (infrequent periods) and amenorrhoea (an absence of periods).1
For a full list of potential side effects, refer to the Summary of Product Characteristics.
If the patient does experience side effects, they should speak to a doctor, pharmacist or nurse. This includes any possible side effects not listed in the contraception package leaflet.
- Bayer Ltd. Mirena® (52 mg intrauterine delivery system levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/mirena-52mg-intrauterine-delivery-system-32902/spc Return to content
Weight gain has been reported as common (can occur in less than 1 in 10 women) in women fitted with Mirena® (52 mg intrauterine delivery system levonorgestrel).1
- Bayer Ltd. Mirena® (52 mg intrauterine delivery system levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/mirena-52mg-intrauterine-delivery-system-32902/spc Return to content
Depression has been reported in fewer than 1 in 10 women fitted with Mirena® (52 mg intrauterine delivery system levonorgestrel).1
There is no clear data to establish whether there is an increased risk of suicidal thoughts and behaviour associated with the use of hormonal contraceptives. Depressed mood and depression are well-known undesirable effects of hormonal contraceptive use. Depression can be serious and is a well-known risk factor for suicidal behaviour and suicide. Women should be advised to contact their physician in case of mood changes and depressive symptoms, including shortly after initiating the treatment.7
- Bayer Ltd. Mirena® (52 mg intrauterine delivery system levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/mirena-52mg-intrauterine-delivery-system-32902/spc Return to content
- European Medicines Agency. PRAC assessment on the use of combined hormonal contraception and suicidality [online]. Available from: https://www.ema.europa.eu/documents/prac-recommendation/prac-recommendations-signals-adopted-1-4-october-2018-prac-meeting_en.pdf Return to content
Mirena® (52 mg intrauterine delivery system levonorgestrel) will affect the patient’s menstrual cycle.8
Patients fitted with the Mirena® coil may experience lighter bleeding or some spotting (light bleeding in between periods) and irregular bleeding during the first 3–6 months after it is fitted.1
Some patients may have prolonged or heavy bleeding or an increase in the frequency of bleeding, usually in the first 2–3 months, before a reduction in blood loss is achieved.1
However, overall patients are likely to have fewer days bleeding in each month and might eventually have no periods at all. This is due to the effect of the hormone (levonorgestrel) on the lining of the womb.1
For women with menorrhagia, Mirena® usually results in lighter periods and can decrease blood loss by up to 94% at 3 cycles and 88% at 6 cycles.8
- Bayer Ltd. Mirena®(52 mg intrauterine delivery system levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/mirena-52mg-intrauterine-delivery-system-32902/spc Return to content
- Reid PC and Virtanen-Kari S. BJOG 2005;112:1121–1125. Return to content
Fertility is restored immediately and conception can occur from the first cycle following removal of the system.11
Studies have suggested that in women who discontinue Mirena® (52 mg intrauterine delivery system levonorgestrel) for planned pregnancy the pregnancy rate at one year is similar to those who do not use contraception.1
- Bayer Ltd. Mirena® (52 mg intrauterine delivery system levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/mirena-52mg-intrauterine-delivery-system-32902/spc Return to content
- Andersson K, et al. Contraception 1992;45:575–584. Return to content
If a patient becomes pregnant while Mirena® (52 mg intrauterine delivery system levonorgestrel) is in place, ectopic pregnancy should be excluded, the system must be removed and termination of the pregnancy should be considered.1
Accordingly, removal of the intrauterine device (IUD) Mirena® or probing of the uterus may also result in spontaneous miscarriage. If the patient wishes to continue the pregnancy and the system cannot be withdrawn, she should be informed about the increased risks and the possible consequences of premature birth to the infant. Such pregnancies should be closely monitored. The patient should be instructed to report all symptoms that suggest complications of the pregnancy, like cramping abdominal pain with fever.1
For more information and a complete list of contraindications, refer to the Mirena® Summary of Product Characteristics.
- Bayer Ltd. Mirena® (52 mg intrauterine delivery system levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/mirena-52mg-intrauterine-delivery-system-32902/spc Return to content
In women of fertile age, Mirena® (52 mg intrauterine delivery system levonorgestrel) is inserted into the uterine cavity within 7 days of the onset of menstruation. It can be replaced by a new system at any time of the cycle.
Mirena® should be inserted during the patient’s menstrual cycle or within 7 days from the beginning of the period.1
Some patients may find the fitting of a Mirena® coil uncomfortable.1 Managing your patient’s expectations with regards to pain is important and many healthcare professionals have found that talking to the patient throughout the fitting helps to reduce anxiety and make them more comfortable. However, it is important to check with your patient if this would be helpful.
The UK National Institute for Health and Care Excellence (NICE) guidelines for long-acting reversible contraceptives (LARC) recommends: 'insertion of an intrauterine device/intrauterine system may cause pain and discomfort for a few hours and light bleeding for a few days, and they should be informed about appropriate pain relief'.12
- Bayer Ltd. Mirena®(52 mg intrauterine delivery system levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/mirena-52mg-intrauterine-delivery-system-32902/spc Return to content
- NICE. Contraception - IUS/IUD [online]. Updated May 2019. Return to content
Some patients may feel pain or have some bleeding during insertion or removal of Mirena®.1
Clinical guidance from the Faculty of Sexual and Reproductive Healthcare in the UK states that there is no evidence from current trials to support the use of topical lidocaine, misoprostol or non-steroidal inflammatory drugs (NSAIDs) for improving ease of insertion or reducing pain during insertion of intrauterine methods.10
- Bayer Ltd. Mirena® (52 mg intrauterine delivery system levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/mirena-52mg-intrauterine-delivery-system-32902/spc Return to content
- Faculty of Sexual and Reproductive Healthcare. Clinical guideline. Intrauterine contraception clinical effectiveness unit [online]. Updated October 2015. Available from: https://www.fsrh.org/standards-and-guidance/documents/ceuguidanceintrauterinecontraception/ Return to content
Recommendations
Reporting adverse events and quality complaints
If you want to report a side effect or quality complaint, please contact your health care professional (e.g. physician or pharmacist) or The Health Products Regulatory Authority, Reports can also be reported directly to Bayer through this link or by emailing directly on adr-reland@bayerhealthcare.com