A low dose, effective contraception without a daily routine
Kyleena® is a low daily hormone dose (12 μg per day over the first year, and averaging 9 μg per day over 5 years) which can be appealing to women.1-3 Independent of user compliance, age and parity, Kyleena® provides highly effective contraception with a 5-year Pearl Index of 0.29.1,2*
*1-year Pearl Index: 0.16 (95% Cls 0.02-0.58). 5-year Pearl Index: 0.29 (95% Cls 0.16-0.50). The failure rate was approximately 0.2% at 1 year.
- Bayer Ltd. Kyleena® Summary of Product Characteristics. Return to content
- Gemzell-Danielsson K, et al. Eur J Obstet Gynecol Reprod Biol, 2017;210:22–28. Return to content
- Mansour D. Int J Women’s Health, 2014;6:367–375. Return to content
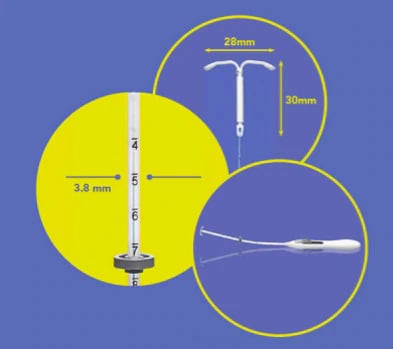
Kyleena®: Smaller T-body and narrower insertion tube than a Mirena
With a 3.8 mm insertion tube:
- Nelson A, et al. Obstet Gynecol, 2013;122:1205–1213. Return to content
- Nelson AL, et al. Expert Rev Clin Pharmacol, 2017;10(8):833–342. Return to content
Which patients could benefit from being prescribed Kyleena?
Dr Deirdre Lundy shares her thoughts on which patients she believes will benefit from being prescribed a Kyleena.
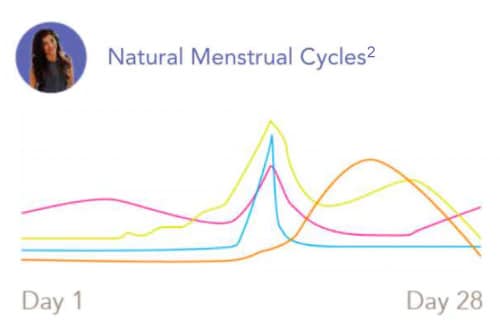
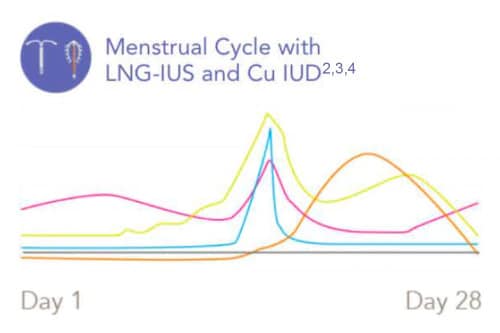
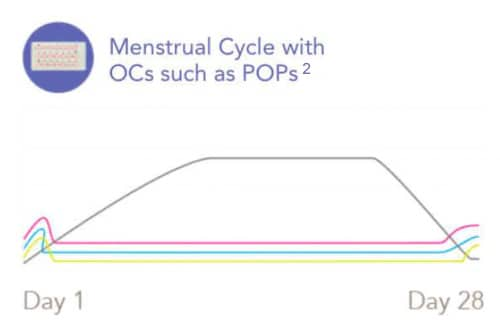
- FSH
- LH
- Oestrogen
- Progesterone
- Progestogen
- Bayer Ltd. Kyleena® Summary of Product Characteristics. Return to content
- Alvergne and Lummaa. Trends in Ecology and Evolution, 2010;25(3):171–179. Return to content
- Apter D, et al. Fertil Steril, 2014;101:1656–1662. Return to content
- ParaGuard® Prescribing Information, Cooper Surgical, 2018.Return to content
Fast facts on Kyleena
In this video, Dr Jane Davis, highlights key facts that are beneficial for healthcare professionals to know when counselling patients about Kyleena.
Duration | 7 minutes 12 seconds
- Gemzell-Danielsson K, et al. Eur J Obstet Gynecol Reprod Biol, 2017;210:22–28. Return to content
Kyleena®: Frequently asked questions
Below you will find answers to some commonly asked questions, which you may find useful when assessing appropriate contraceptive options for patients or counselling patients on contraception choice and Kyleena® (19.5 mg intrauterine delivery system levonorgestrel).
Kyleena® (19.5 mg intrauterine delivery system levonorgestrel) is an intrauterine system (IUS) indicated as a contraceptive for the prevention of pregnancy for up to 5 years.1
Of the IUS with a 5 or 8 year contraception license, Kyleena® has the smallest T frame (28 x 30 mm) and narrowest insertion tube (3.8 mm).1,2
In a multicentre study, a survey showed that 48% of women aged 18-44, and in particular young women (18-24 - 57%) forgot to take their contraceptive pill in the last 3 months. Kyleena® can be beneficial for women who struggle to adhere to contraceptive compliance, e.g. taking the pill at the same time every day.3
In the same survey, 87% of women mentioned that a method not requiring daily, weekly or monthly dosing would make things easier and 80% would consider switching contraceptives to minimise oestrogen exposure.3
- Bayer Ltd. Kyleena® 19.5 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics [online]. Available from: https://www.medicines.ie/medicines/kyleena-19-5-mg-intrauterine-delivery-system-32621/spc Return to content
- Gemzell-Danielsson K, et al. PLoS One 2015;10:e0135309. doi: 10.1371/journal.pone.0135309. Return to content
- Hooper DJ. Clin Drug Investig 2010;30:749–763. Return to content
A recent study of more than 6,000 women showed that 73% across all age ranges (18–49) would consider long-acting reversible contraception (LARC) if provided with substantial information from their healthcare professional on this method (compared with 38% estimated by healthcare professionals).4
In general, patients are more positive about the idea of an LNG-IUS such as Kyleena® after they receive education about them vs those who have not. This highlights the importance of effective counselling to increase awareness and knowledge.5
A patient may feel reticent to have a Kyleena® (19.5 mg intrauterine delivery system levonorgestrel) inserted, this could be due to the following myths and misperceptions:
- 'Fitting and removal will be painful'. 80% of women perceive the placement procedure as painful15
- Some patients may feel pain or have some bleeding during insertion or removal1
- 'The IUS will perforate and end up somewhere other than my uterus without me knowing'.
- Perforation occurs in less than 1 in 1000 women and can be detected by severe pelvic pain and continued heavy bleeding for more than a few weeks after insertion16
- 'I will suffer years of irregular bleeding'
- The chance of irregular bleeding is highest in the first 3-6 months.
Women have other perceptions of IUS which it is important to counsel them around:
- 63% of women consider having low/no hormones to be important when choosing contraception15
- 30% of women are opposed to having something like a hormonal coil inserted in their body15
- 37% of women feel they don’t know enough about hormonal coils15
However, a study by Whitaker et al showed that adolescents and young women reported a positive attitude towards intrauterine contraceptives before and after a 3-minute educational intervention counselling tool. This included information about intrauterine contraception (IUC) effectiveness, insertion and removal process, risks, benefits, costs, effect on fertility, menstrual effects, length of use, similarities and differences between types of IUC available. Attitudes before and after the education intervention were assessed by questionnaire.5
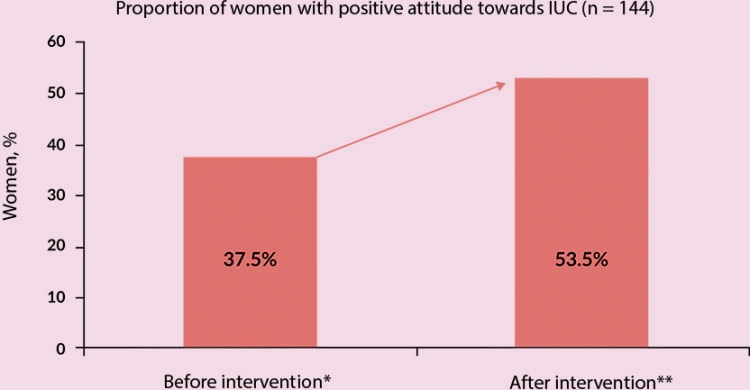
*(Women who had heard of the IUD previously, n = 57)
**(All women, n = 144)
- Bayer Ltd. Kyleena® 19.5 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/kyleena-19-5-mg-intrauterine-delivery-system-32621/spc Return to content
- Merki-Feld GS, et al. Eur J Contracept Reprod Health Care 2018;23:183–193. Return to content
- Whitaker A, et al. Contraception 2008;78:211–217. Return to content
- PULSE survey 2018 UK. Return to content
- gov.uk. Intrauterine contraception: uterine perforation—updated information on risk factors [online]. Updated 26 June 2015. Available from: https://www.gov.uk/drug-safety-update/intrauterine-contraception-uterine-perforation-updated-information-on-risk-factors. Return to content
Kyleena® contains 19.5 mg levonorgestrel and has a mainly local progestogenic effect in the uterine cavity.1
Interactions can occur with medicinal products that induce microsomal enzymes, which can result in increased clearance of sex hormones, for example:1
- Medicines used to treat epilepsy (e.g. phenytoin and topiramate)
- Sedatives (called barbiturates)
- Anticonvulsants (e.g. primidone and carbamazepine)
- Certain antibiotics (e.g. rifampicin and possibly also oxcarbazepine)
- Antifungal medicines (e.g. griseofulvin)
- Products containing St John's wort (a herbal remedy)
It is advised that prescribing information of concomitant medications should be consulted to identify potential interactions. For a full list of medicinal interactions and contraindications, refer to the Summary of Product Characteristics.
- Bayer Ltd. Kyleena® Kyleena® 19.5 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics [online]. Available from: https://www.medicines.ie/medicines/kyleena-19-5-mg-intrauterine-delivery-system-32621/spc Return to content
The majority of patients experience changes in menstrual bleeding pattern after insertion of Kyleena® (19.5 mg intrauterine delivery system levonorgestrel). Women can experience shorter, lighter bleeds and can experience amenorrhoea over 5 years. Very common side effects (more than 1 in 10 women) include:1,6
- headache
- abdominal/pelvic pain
- acne/greasy skin
- bleeding changes including increased and decreased menstrual bleeding, spotting, infrequent periods and absence of bleeding
- ovarian cysts
- inflammation of the external genital organs and vagina (vulvovaginitis)
- Common side effects (up to 1 in 10 women) include:6
- depressed mood/depression
- migraine
- feeling sick (nausea)
- upper genital tract infection
- painful menstruation
- breast pain/discomfort
- device expulsion (complete and partial)
- hair loss
- genital discharge
For a full list of potential side effects, refer to the Summary of Product Characteristics and Patient Information Leaflet .
Educational Risk Minimisation Materials can be downloaded here to help reduce the risks associated with using Kyleena®.
If the patient does experience side effects, they should speak to a doctor, pharmacist or nurse. This includes any possible side effects not listed in the contraception package leaflet.
- Bayer Ltd. Kyleena® 19.5 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/kyleena-19-5-mg-intrauterine-delivery-system-32621/spc Return to content
- Bayer Ltd. Kyleena® 19.5 mg intrauterine delivery system (levonorgestrel): Patient Information Leaflet. Available from: https://www.medicines.ie/medicines/kyleena-19-5-mg-intrauterine-delivery-system-32621/patient-info Return to content
Weight gain has been reported as common (can occur in less than 1 in 10 women) in women fitted with Kyleena (19.5mg intrauterine delivery system levonorgestrel)1
- Bayer Ltd. Kyleena® 19.5 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/kyleena-19-5-mg-intrauterine-delivery-system-32621/spc. Return to content
For Mirena® (52 mg intrauterine delivery system levonorgestrel), very common undesirable effects (occurring in more than 10% of users) include uterine/vaginal bleeding, such as spotting, oligomenorrhoea and amenorrhoea. Undesirable effects are more common during the first months after the insertion and subside during prolonged use.14
For Kyleena® (19.5 mg intrauterine delivery system levonorgestrel), very common undesirable effects include headaches, abdominal/pelvic pain, acne/seborrhoea, ovarian cysts, vulvovaginitis and bleeding changes including increased and decreased menstrual bleeding, spotting, infrequent bleeding and amenorrhoea. Over time, the frequency of amenorrhoea and infrequent bleeding increases, and the frequency of prolonged, irregular and frequent bleeding decreases.1
For further information on Kyleena® and Mirena® please visit the Summary of Product Characteristics.
- Bayer Ltd. Kyleena® Kyleena® 19.5 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/kyleena-19-5-mg-intrauterine-delivery-system-32621/spc Return to content
- Bayer Ltd.. Mirena® 52 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/mirena-52mg-intrauterine-delivery-system-32902/spc Return to content
Effects on the menstrual bleeding pattern are expected in most users of Kyleena®.1
Irregular bleeding and spotting are common in the first months of use. Thereafter, the strong suppression of the endometrium results in the reduction of the duration and volume of menstrual bleeding. Scanty flow frequently develops into oligomenorrhoea or amenorrhoea.1
Patients may have bleeding and spotting between menstrual periods, especially during the first months.
Overall, patients are likely to have a gradual reduction in the amount and number of days of bleeding each month. Some women eventually find that periods stop altogether,7 with 23% experiencing amenorrhoea at the end of Year 5.1
When the intrauterine system (IUS) is removed, the patient’s menstrual cycle should return to normal.1
- Bayer Ltd. Kyleena® 19.5 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/kyleena-19-5-mg-intrauterine-delivery-system-32621/spc Return to content
- Nelson A, et al. ObstetGynecol 2013;122:1205–1213. Return to content
Both Mirena® and Kyleena® affect patients’ bleeding patterns.
A Phase II study compared the IUSs Jaydess®▼ (13.5 mg intrauterine delivery system levonorgestel), Kyleena® and Mirena® (with initial in vitro release rates of 12 μg/d, 16 μg/d and 20 μg/d respectively) and found that the bleeding profiles were similar in all groups, although total bleeding and spotting days decreased with increasing levonorgestrel dose.9
- Gemzell-Danielsson K, et al. FertilSteril 2012;97:616–622.1–3. Return to content
The contraceptive efficacy of Kyleena® (19.5 mg intrauterine delivery system levonorgestrel) has been evaluated in a clinical study with 1,452 women aged 18–35 including 39.5% (574) nulliparous women of whom 84.0% (482) were nulligravid using Kyleena®. The 1-year Pearl Index was 0.16 (95% confidence interval 0.02–0.58) and the 5-years Pearl Index was 0.29 (95% confidence interval 0.16–0.50). The failure rate was approximately 0.2% at Year 1 and the cumulative failure rate was approximately 1.4% at Year 5.1
It is therefore, uncommon for a patient to become pregnant while using Kyleena®, however, approximately half of the pregnancies that occur during Kyleena®-use are likely to be ectopic.1
The overall incidence of ectopic pregnancy in Phase II and III clinical trials with Kyleena® was 0.2 per 100 women-years.1
The possibility of an ectopic pregnancy must be carefully considered and evaluated. An ectopic pregnancy should be considered in the case of lower abdominal pain, especially in connection with missed periods or if an amenorrhoeic woman starts bleeding.1
- Bayer Ltd. Kyleena® 19.5 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/kyleena-19-5-mg-intrauterine-delivery-system-32621/spc Return to content
The use of a levonorgestrel-releasing intrauterine delivery system does not alter the course of future fertility. Upon removal of the intrauterine system, women return to their normal fertility.1
- Bayer Ltd. Kyleena® 19.5 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/kyleena-19-5-mg-intrauterine-delivery-system-32621/spc Return to content
It is uncommon for a woman to become pregnant while using Kyleena®, however, approximately half of the pregnancies that occur during Kyleena®-use are likely to be ectopic. If a patient does become pregnant while using Kyleena®, ectopic pregnancy should be excluded and timely removal of the system is recommended, since any intrauterine contraceptive left in situ may increase the risk of miscarriage and preterm labour.
Women considering Kyleena® should be counselled on the signs, symptoms and risks of ectopic pregnancy on an individual basis as an ectopic pregnancy may impact future fertility.
Women with a previous history of ectopic pregnancy, tubal surgery or pelvic infection carry an increased risk of ectopic pregnancy.
If the patient wishes to continue the pregnancy and the system cannot be withdrawn, she should be informed about the risks and the possible consequences of premature birth of the infant. The course of such a pregnancy should be closely monitored.
The patient should be instructed to report all symptoms that suggest complications of the pregnancy, like cramping abdominal pain with fever.1
For more information and a complete list of contraindications, refer to the Kyleena® Summary of Product Characteristics
- Bayer Ltd.. Kyleena® 19.5 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/kyleena-19-5-mg-intrauterine-delivery-system-32621/spc. Return to content
Insertion and removal of Kyleena® (19.5 mg intrauterine delivery system levonorgestrel) may be associated with some pain and bleeding. The procedure may precipitate a vasovagal reaction (e.g. syncope, or a seizure in an epileptic patient).1
The UK National Institute for Health and Care Excellence guidelines for long-acting reversible contraceptives (LARC) recommends: ‘insertion of an IUS/IUD may cause pain and discomfort for a few hours and light bleeding for a few days, and patients should be informed about appropriate pain relief’.17
Clinical guidance from the Faculty of Sexual and Reproductive Healthcare in the UK states that there is no evidence from current trials to support the use of topical lidocaine, misoprostol or non-steroidal inflammatory drugs (NSAIDs) for improving ease of insertion or reducing pain during insertion of intrauterine methods. A discussion should be had on an individual basis on what pain relief may be required.
Managing your patient’s expectations with regards to pain is important and many healthcare professionals have found that talking to the patient throughout the fitting helps to reduce anxiety and makes them more comfortable. However, it is important to check with your patient if this would be helpful.13
- Bayer Ltd. Kyleena® 19.5 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/kyleena-19-5-mg-intrauterine-delivery-system-32621/spc Return to content
- FSRH clinical guidance. Intrauterine contraception clinical effectiveness unit April 2015 [online]. Updated October 2015. Available from: https://www.fsrh.org/standards-and-guidance/documents/ceuguidanceintrauterinecontraception/ Return to content
- NICE. Contraception—IUS/IUD [online]. Updated January 2019. Return to content
Kyleena® (19.5 mg intrauterine delivery system levonorgestrel), has a small T-frame (28 x 30 mm) placed using an inserter with narrow insertion tube (3.8 mm).2
Kyleena® may be suitable for women who would prefer a lower dose of levonorgestrel and do not require the added endometrial protection during oestrogen replacement therapy or treatment for menorrhagia. For an intrauterine delivery system that is licensed for these indications, refer to information on Mirena® (52 mg intrauterine delivery system levonorgestrel).
- Gemzell-Danielsson K, et al. PLoS One 2015;10:e0135309. doi: 10.1371/journal.pone.0135309. Return to content
Kyleena® and Jaydess®▼ (13.5 mg intrauterine delivery system levonorgestrel) are smaller (28 x 30 mm) than Mirena® (32 x 32 mm).
The IUS, Jaydess®▼, contains 13.5 mg levonorgestrel, Kyleena®, contains 19.5 mg levonorgestrel, a lower dose than Mirena®, containing 52 mg levonorgestrel.1,14,18
Kyleena® is indicated as contraception for up to 5 years, compared with Jaydess®▼, which is effective for 3 years.1
For more information about Bayer IUS please visit the Risk Minimisation Materials.
- Bayer Ltd. Kyleena® 19.5 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/kyleena-19-5-mg-intrauterine-delivery-system-32621/spc. Return to content
- Bayer Ltd.. Mirena® 52 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/mirena-52mg-intrauterine-delivery-system-32902/spc . Return to content
- Bayer Ltd. Jaydess®▼ (13.5 mg intrauterine delivery system levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/jaydess-13-5-mg-intrauterine-delivery-system-32547/spc Return to content
If the patient wishes to continue using the same method, a new system can be inserted at the same time (removal should be carried out within 7 days of the onset of menstruation), in which case no additional protection is required provided the woman is experiencing regular menses.1
- Bayer Ltd. Kyleena® 19.5 mg intrauterine delivery system (levonorgestrel): Summary of Product Characteristics. Available from: https://www.medicines.ie/medicines/kyleena-19-5-mg-intrauterine-delivery-system-32621/spc. Return to content
Recommendations
Reporting adverse events and quality complaints
If you want to report a side effect or quality complaint, please contact your health care professional (e.g. physician or pharmacist) or The Health Products Regulatory Authority, Reports can also be reported directly to Bayer through this link or by emailing directly on adr-reland@bayerhealthcare.com